-
Address: Suite 4 (level 1), 52 Hatherley Parade, Winthrop, WA 6150.
-
Phone: 08 9332 2455
-
Email: reception@waurology.com.au

TURBT
WHAT IS TURBT?
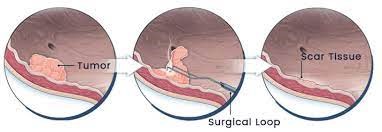
The full form of TURBT is Trans-Urethral Resection of Bladder Tumour. It refers to the surgical removal of a tumour or growth in the bladder. It is done endoscopically.
WHAT IS THE INDICATION FOR A TURBT?
The predominant reason for a TURBT is when a diagnosis of a bladder tumour has been made. The bladder tumour would have been confirmed via a flexible cystoscopy examination prior to the TURBT.
WHAT DOES A TURBT INVOLVE?
A TURBT is done in hospital under a full general anesthetic. It commonly requires an overnight and in some cases 2 to 3 days stay in hospital.
You will be asked to fast for 6 hours prior to your procedure. Once you arrive at the hospital the nurses will admit and get you prepared for the procedure.
You will be taken to the operating room once your turn for the procedure has arrived. The anesthetist will give you medications to get you off to sleep completely. Once you are asleep Dr Vasudevan will clean the required area with anti-septic solution such as betadine. Once this is done an instrument called a cystoscope will be inserted through the urethra and into the bladder to get an assessment of the location and distribution of the bladder tumour. Once the preliminary assessment has been done an instrument called a resectoscope is inserted via the urethra and using a device called a loop diathermy the bladder tumour is resected completely. Deeper samples of the bladder muscle are also taken to assess the depth of penetration of the bladder tumour.
All the resected specimen is sent of the laboratory for assessment under the microscope.
Once the bladder tumour has been fully resected another device called diathermy ball is used to seal of any blood vessels that may be bleeding. Once this has been completed a catheter is inserted into the bladder and an irrigation of the bladder is commenced which is kept running overnight.
Once the procedure has been completed you will be woken up and transferred to the recovery area where you will be kept under observation till you are fully awake. Once you are awake, you will be transferred to the ward where the nurses will be monitoring your bladder irrigation overnight.
The following morning Dr Vasudevan will review you and if the bladder irrigation appears clear, the catheter will be removed. You will be kept in hospital till you have passed urine 2 to 3 times to ensure that you are emptying your bladder properly. Once you have done so you will be discharged from hospital.
WHAT CAN YOU EXPECT AFTER A TURBT?
When you get home, while you are free to do your normal daily chores, it is advisable not to do strenuous activities and exercise for 2 to 3 weeks.
You may experience the following after a TURBT.
- Occasional show of blood in the urine- it is normal for your urine to have tinges of blood after the procedure. This is due to the raw area in your bladder. Once the raw area has completely healed which can take 3 to 4 weeks the blood in the urine will resolve.
- Frequent and urgent urination – this is normal and is due to the raw area in the bladder, which will resolve once the resected area has healed.
- Burning sensation when passing urine – which will resolve once the raw area has healed.
WHAT ARE POSSIBLE COMPLIACTIONS OF A TURBT?
Possible complications from a TURBT include:
- Urine infection (UTI) – while Dr Vasudevan will take all precautions prior to and during surgery to minimize urinary infections, if you feel feverish or unwell several days after the operation, please inform Dr Vasudevan who will arrange for your urine to be tested for a UTI. If an infection is present antibiotics will be prescribed.
- Persistent and heavy bleeding – if you notice prolonged and heavy bleeding with clot formation please return back to hospital. A catheter will need to inserted and a bladder irrigation will need to be started. In most cases the bleeding will resolve with irrigation, however in some cases a return back to theatre may be needed to cauterize (seal) off any blood vessels that may be bleeding.
- Perforation of bladder – This is when an inadvertent hole is made in the bladder. If this does occur it will be recognized during the operation and in most cases leaving the catheter in for a few extra days will allow the body to heal and close the hole by itself. However, in extremely rare situations a bigger procedure may be needed to close the hole in the bladder.
- Scar in urethra – As a TURBT is done via the urethra, it is rare but possible that a scar may form in the urethra causing a weak urine flow. This mostly occurs a few months after the completion of surgery. If this did occur further surgery may be need to rectify the problem.
FOLLOW-UP WITH DR VASUDEVAN
Dr Vasudevan will review you in his office 3 weeks after the procedure to ensure that you are recovering appropriately and also to discuss the pathology results of the resected bladder tumour.
Depending on the results Dr Vasudevan will arrange subsequent treatment if needed and / or ongoing surveillance of your bladder.
